Singye Wangmo1 , Namgay Lhamo2
, Namgay Lhamo2 , Tashi Tenzin3
, Tashi Tenzin3 , Ugyen Wangchuk4
, Ugyen Wangchuk4
1Department of Lay-Nga, National Traditional Medicine Hospital, Thimphu, Bhutan
2Faculty of Traditional Medicine, Khesar Gyalpo University Medical Sciences of Bhutan, Thimphu, Bhutan
3Faculty of Postgraduate Medicine, Khesar Gyalpo University Medical Sciences of Bhutan, Thimphu, Bhutan
4Department of Acupuncture, National Traditional Medicine Hospital, Thimphu, Bhutan
Corresponding author: Singye Wangmo, Department of Lay-Nga, National Traditional Medicine Hospital, Thimphu, Bhutan
Email: singyewangmo@nms.gov.bt
DOI: https://doi.org/10.47811/bsj.0002050301
Copyright © 2025 Bhutan Sorig Journal published by the Faculty of Traditional Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan.
This is an open access article under the CC BY-NC-ND license.
ABSTRACT
Introduction: Skin disease is one of the most common diseases treated at the National Traditional Medicine Hospital in Bhutan. Since the establishment of Inpatient Department in 2018, Shel (purgation) with Tshawa-suum paste application is used as the treatment for Langshu skin disorders. This study was conducted to assess the effectiveness of Shel with Tshawa-suum paste on Langshu.
Methods: It was an observational study conducted among patients admitted with Langshu at National Traditional Medicine Hospital, Thimphu, Bhutan. A structured questionnaire was used to collect the sociodemographic details of the patients and Eczema Area and Severity Index (EASI) score was used to assess the severity and extent of skin lesions. Patients were assessed at three time points: before the treatment, after 7 days of treatment and on day 30 when the patients reported for follow-up care.
Results: The mean age of the patients (±SD) was 38.81 (±17.63) years and 57.14% were male. The majority of the patients were farmers (42.43%). At baseline, there were 6 patients with very severe Langshu lesion, 44 with severe and 20 with moderate condition. By day 30, only 3 had severe, 34 had mild and 33 had moderate condition. The study found statistically significant reduction in the mean EASI score from 30.12 on Day 0 to 17.25 on Day 7 and 8.46 on Day 30 (p < 0.001).
Conclusions: This study shows that the use of Shel with Tshawa-suum paste resulted in decrease in size and severity of Langshu skin lesions.
Keywords: Alternative medicine; Dermatology; Purgatives; Skin disease; Traditional medicine
INTRODUCTION
In Bhutan, the Ministry of Health reported skin disorders as the second leading cause of morbidity seen across hospitals in the country [1]. In Sowa Rigpa, Bhutanese Traditional Medicine, skin diseases are collectively known as pagney. It is one of the top ten diseases treated at the National Traditional Medicine Hospital (NTMH). Sowa Rigpa classifies skin diseases into nine categories: sha tra, zerpa, zakong, shuwa, sin thor, ngo shig, ngo khep, chema and langshu [2]. Langshu is the most commonly treated skin diseases at NTMH. It literally translates as ox-scab, where the diseased skin looks like the scab on ox’s neck formed as a result of abrasion of yoke. Langshu is characterized by various signs and symptoms including itching (za thruk lang pa), skin thickening (pagpa thukppo), rough (tsubpa) and leathery (langhi nya tabu), dark coloured skin and redness (pagdhog marmuk) [3].
Treatment methods for skin diseases available at NTMH include: oral medicines, langduk (herbal steaming), serkhap (golden needle therapy), tar (bloodletting), Shel (purgation) and Tshawa-suum paste (herbal paste). Among the various methods of treatments, Shel (purgation) with topical application of Tshawa-suum paste (herbal paste) was started in 2018, with the establishment of an In-patient Department (IPD). While anecdotal feedback from most of the patients were positive about the use of this therapy, some patients are sceptical about the effectiveness of the treatments.
A systemic review done in China where seven randomized control trails were included comparing Chinese herbal medicine and placebo reported that Chinese herbal medicine was found effective in improving the symptoms and severity of atopic dermatitis [4]. Similar study using Ayurvedic Medicine in India also found the purgation with local application of the herbal medicine was effective in reducing symptoms of Vicharchika Kushtha (eczema) [5]. However, no studies were found in Bhutan to assess the treatment outcome of Bhutanese Traditional Medicine on skin disease. Therefore, this study aimed to assess the outcome of the Shel with Tshawa-suum paste on the skin disease, Langshu.
METHOD
Study design
This was an observational study. It involved the patients with Langshu undergoing the therapy of Shel with Tshawa-suum paste in the In-Patient Department at NTMH, Kawajangsa, Thimphu, from November 2020 to October 2021.Study setting
National Traditional Medicine Hospital is the apex traditional medicine hospital in Bhutan. Services include invasive therapies such as bloodletting, golden needle therapy, moxibustion, and acupuncture; non-invasive therapies such as herbal bath, herbal steaming, body massage and hot compression.
In 2018 a ten-bedded In-Patient Department was established and the services provided in the ward were mainly lay-nga therapies. The lay-nga is an eliminative therapy in Sowa Rigpa that involves five actions which helps in detoxification, cleansing and rejuvenation of the body and mind [6]. The therapies include shel (purgation), chug (emesis), namen (nasal cleansing), jamtse (mild enema) and nerukha (strong enema). Skin disorder is the most common reason for admission to ward.
Study population and sample size
All patients with Langshu who came to avail Shel treatment in NTMH were invited to participate in the study. However, patients with diabetes and hypertension and those on allopathic medicines for long-standing co-morbid conditions were excluded. Among 75 patients with Langshu included for this study, five patients dropped out of this study due to challenges in follow-up and COVID-19 pandemic travel restrictions.
Diagnosis and treatment of Langshu
The diagnosis of the disease (Langshu) was confirmed by two specialist drungtshos with decision by consensus. The diagnosis is based on the clinical signs and symptom of the Langshu as per Sowa Rigpa text which includes erythema, papulation, excoriation and lichenification [3].
As per the Sowa Rigpa text, Langshu can be treated well by Shel with the application of Tshawa-suum paste. Shel is the procedure wherein body toxins are flushed through controlled purgation. Sowa Rigpa explains that Shel is the best treatment to overcome accumulation of excess Thripa (bile), which would otherwise give rise to diseases such as gastritis, abscess, liver disorders, diabetes and skin disorders [3]. Tshawa-suum is composed of five herbal ingredients chetsha (Ranunculus brotherusi), emong (Clematis acutangula), supka (Anemone griffithii), muzi (Sulphur navitum), dongroe (realgar) and phagtshel (pig lark) which are prepared into a paste and applied on the affected area, along with the Shel therapy [7].
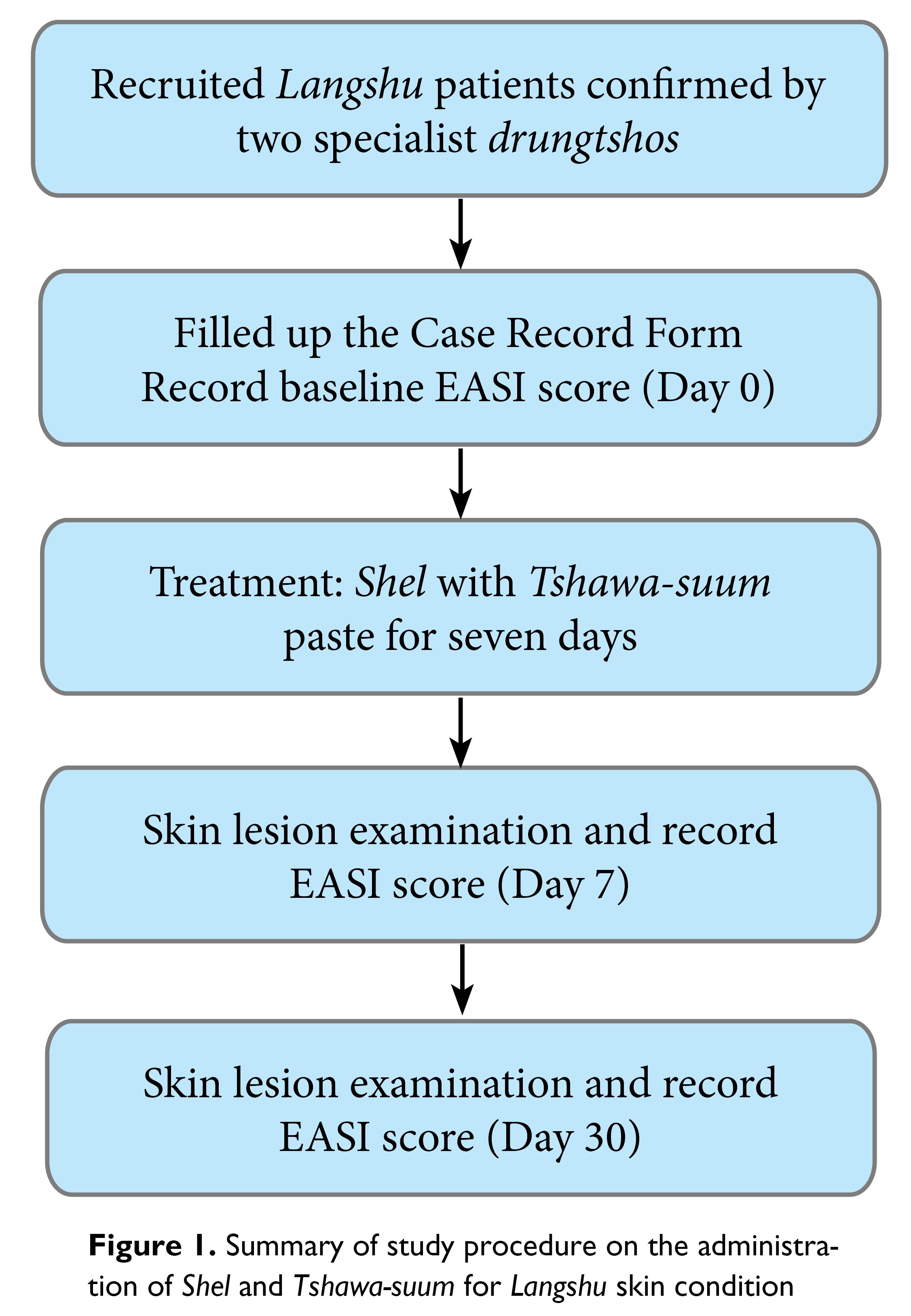
On the day of admission, information of the patients related to skin diseases were recorded. The body surface area affected by Langshu were recorded on the case record form. The sampled patients were given the usual treatment using Shel with Tshawa-suum paste as per the standard treatment protocols approved by the hospital. The treatment was provided by the drungtshos and menpa on duty in the ward, while the investigator remained as a passive observer. The skin lesion of the patients was assessed for the second time on day 7 and recorded. The final assessment of the skin lesion was conducted on day 30, when the patients reported for the follow-up examination.
The treatment included topical application of Tshawa-suum paste on their affected skin once daily for seven days. The paste was applied evenly and kept overnight and were asked to wash away in the morning. Simultaneously, the patients were prepared for the Shel therapy with pre-therapy preparation for five days. The pre-therapy/procedures such as consumption of zhun-maar (processed butter) and other dietary advices were as per the guidelines of Shel therapy.
On the fifth day, the Shel therapy was conducted where the patients were given Shel medicine at 6.00 am. The patients were given 250 mL of jamtsa chukuel, a salty water every fifteen minutes. On average, after thirty minutes the patients started emptying their bowel frequently. The drungtsho and menpa on duty had monitored the patients and kept the records of the frequency and the colour of the stool, based on which the decision was taken to continue or to stop the Shel medication.
The Shel procedure was
continued until the stool colour appeared like water with more frequency of
visits to the toilet. On an average, after the tenth visit to toilet, the patients were given the dreyoe sumthang,
a medicine to stop the Shel. Patients were advised to consume easily digestible diet and avoid strenuous
behaviours after the treatment and was monitored for a day [8]. The details of patient flow and data collection
procedure is shown in Figure 1.
Study tool
The questionnaire consisted of two parts: Part A collected the demographic profile and Part B recorded the skin lesion of Langshu using Eczema Area and Severity Index (EASI) scoring table. Given the lack of an appropriate tool in Traditional Medicine, the EASI score was used as a substitute. EASI score is the most reliable among the other several outcome measures for treatment follow in patients with atopic dermatitis [9]. The EASI score comprises of the percentage of body surface area involvement, severity of skin lesions compared to a standard atlas and the generation of EASI score based on the metrics given in the tool. The EASI score ranged from 1 to 72 and the scores were categorized as 1 – 7 = mild, 7.1 – 21 = moderate, 21.1 – 50 = severe and 50.1 – 72 = very severe.
Data entry and analysis
Data collected were entered twice and validated using the EpiData Entry version 3.1 and analysed using EpiData Analysis version 2.2.2.183 (EpiData Association, Odense, Denmark). Socio-demographic characteristics were described using frequencies and proportion for categorical variables and mean with standard deviation (SD) for continuous variables. For inferential statistics, paired t-test was used to compare the mean EASI score for pre- and post-intervention of each patient. Repeated measure ANOVA test was conducted to compare the mean EASI score between Day 0, Day 7 and Day 30.
Ethics approval
Ethics approval for this study was granted by Interim Institutional Review Board, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan, vide approval no. INTERIM IRB/PO20/022/ 454 dated 24 September 2020. Administrative clearance was obtained from the Medical Superintendent of NTMH. The permission to use EASI score tool was obtained from Wiley Global Permission. Informed consent was obtained from all the patients before the collection of data.
RESULTS
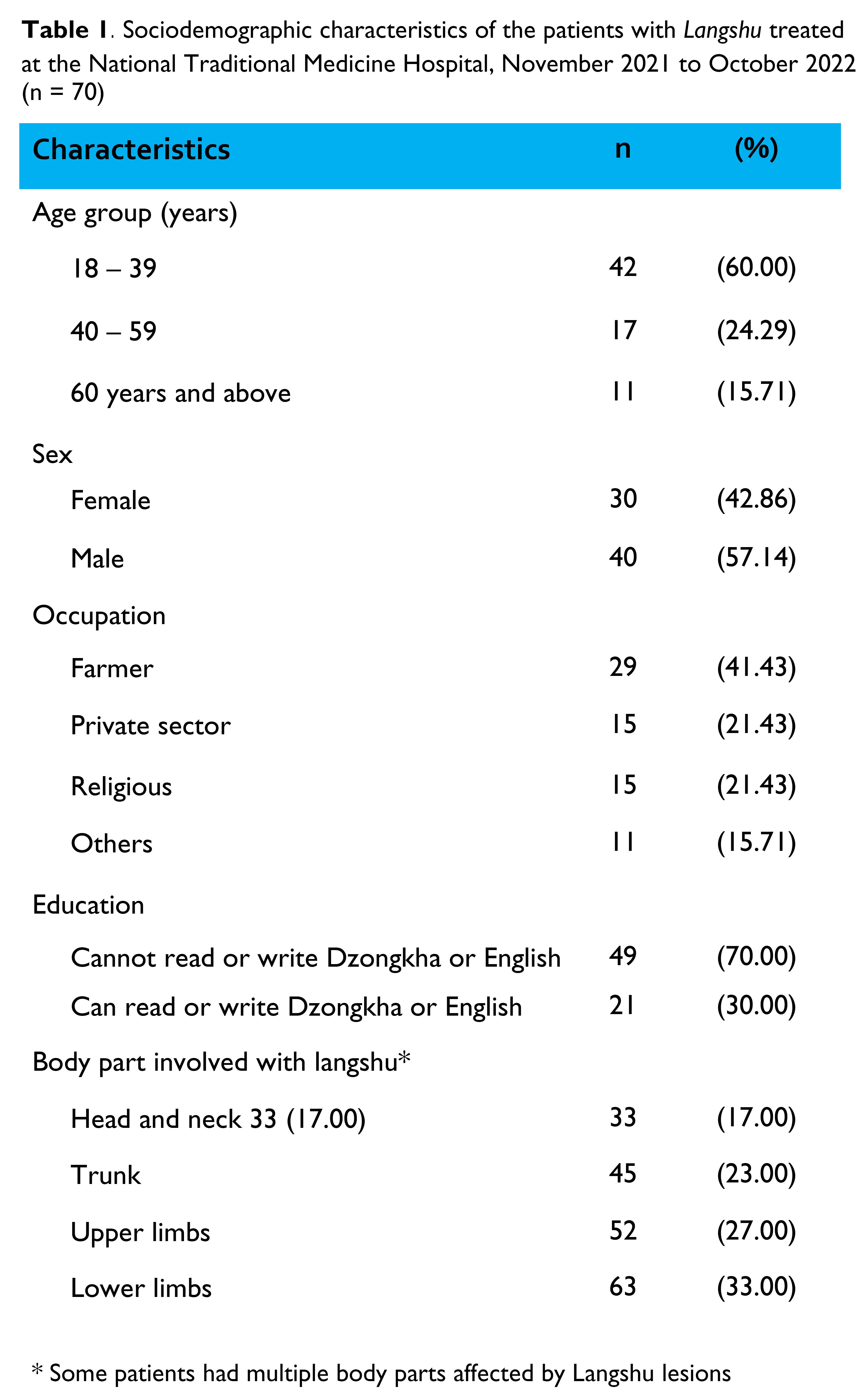
There were 70 patients with Langshu, 57.14% were male and the majority of the patients were literate. The mean age of the patients (±SD) was 38.81 (±17.63) years. The basic characteristics of the patients are given in Table 1. The majority of the patients had Langshu on lower limbs followed by upper limbs and trunk.
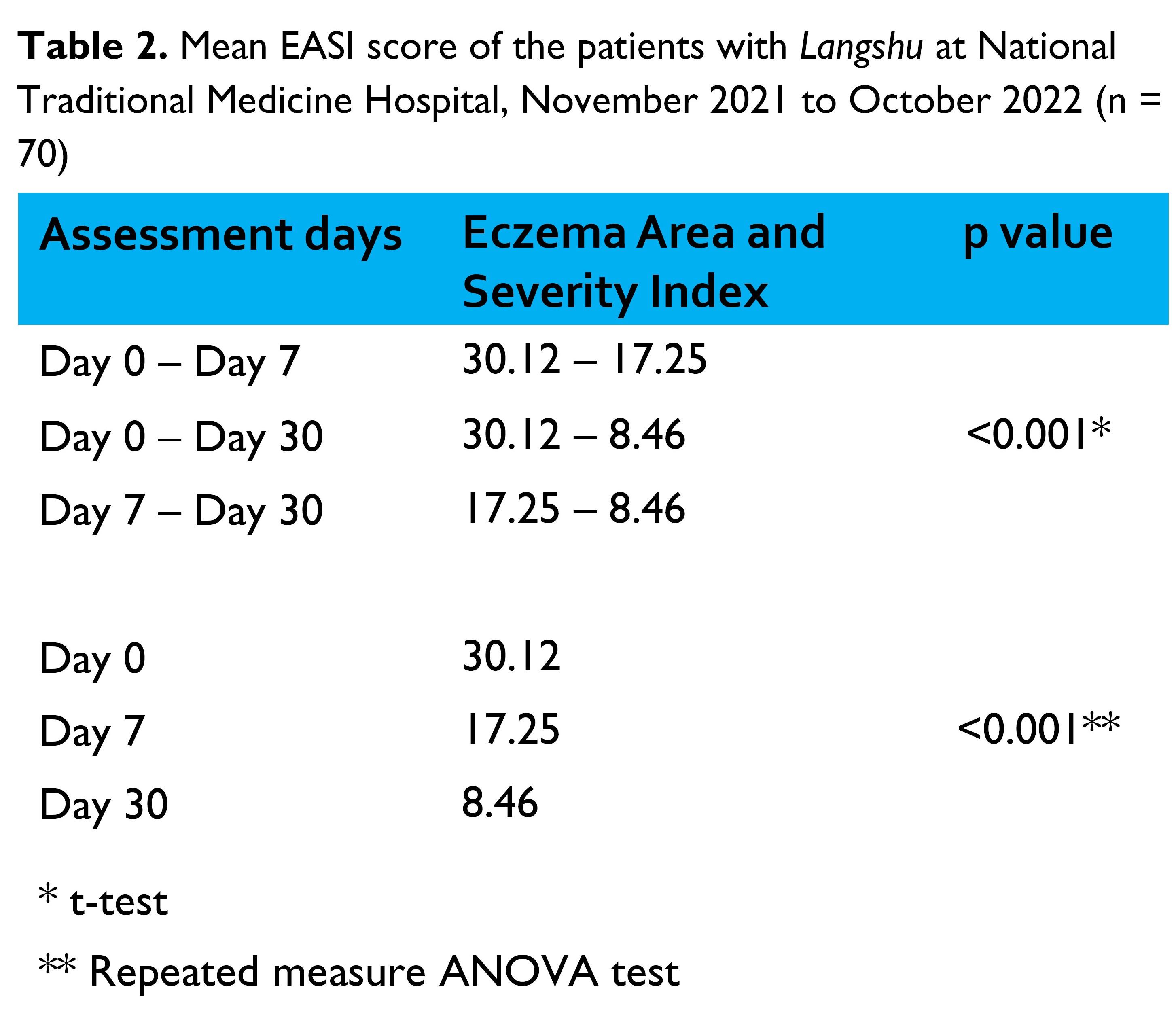
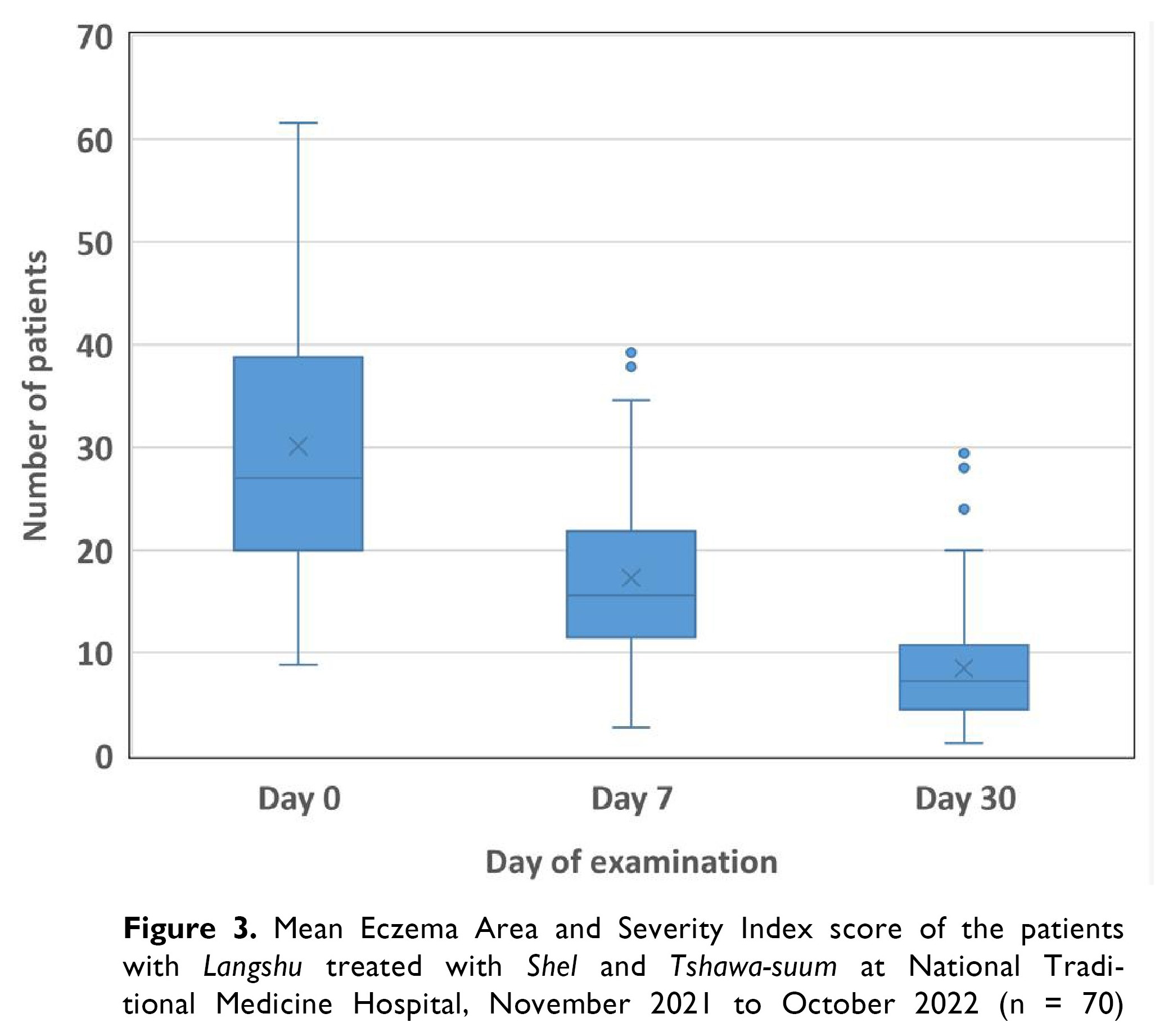
Assessment of EASI score
On Day 0, majority of the patients fell in severe and very severe (n = 50) categories. After 7 days of treatment, patients migrated to moderate and severe (n = 65) categories. On Day 30 follow up, 67 many patients had mild and moderate condition. On Day 0, 6 patients had very severe Langshu lesions, while there were no patients with very severe condition on Day 30 (Figure 2).
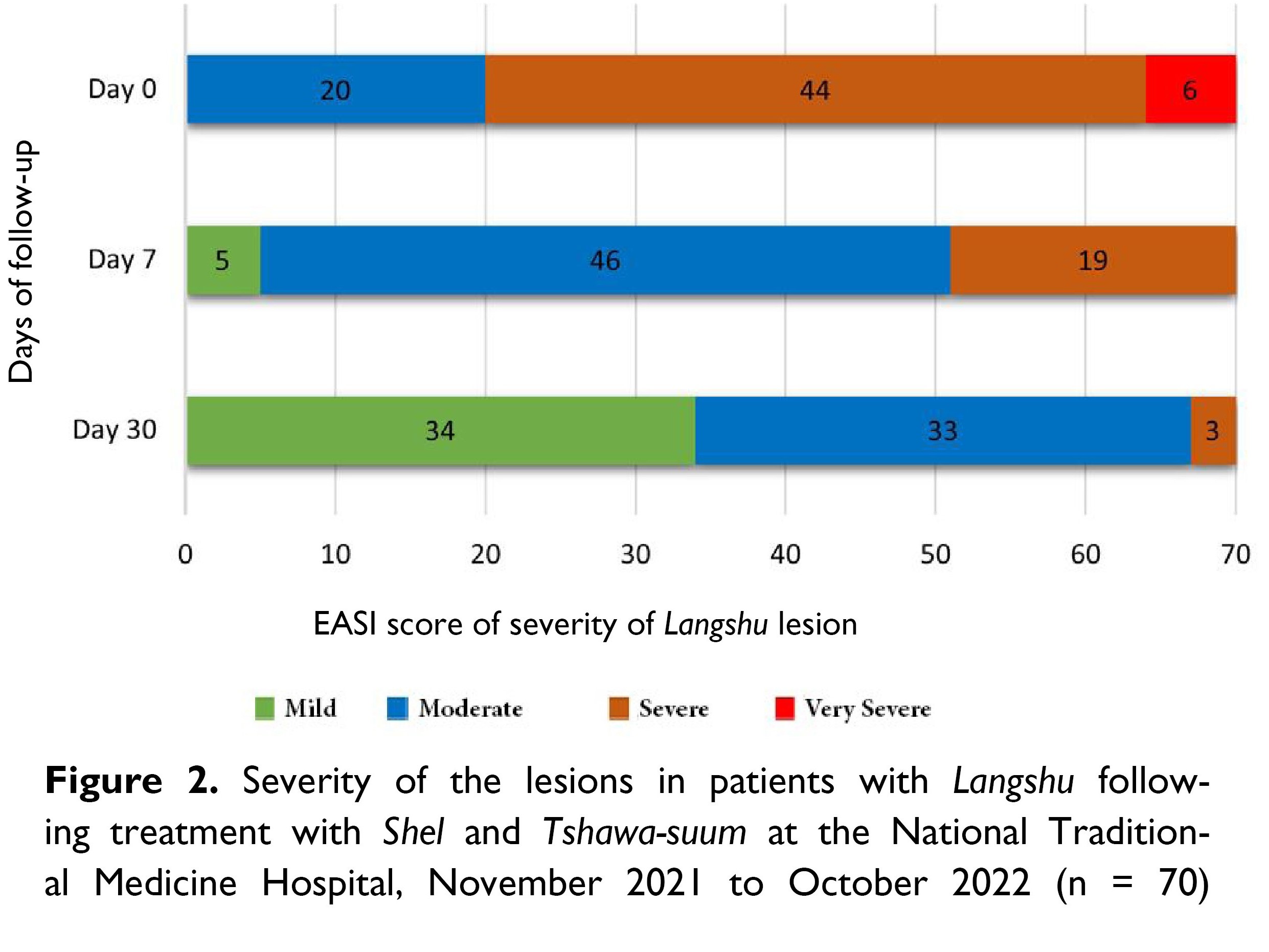
Over the period of treatment, there was serial reduction in the mean EASI score from 30.12 at baseline to 17.25 on Day 7 and 8.46 on Day 30, p < 0.001, as shown in Table 2 and Figure 3.
As shown in Figure 4 and 5, there was marked improvement in terms of reduction of the size of lesion, redness and skin patches.


DISCUSSION
This study found that there was a significant decrease in the size of langshu skin lesions using Bhutanese Traditional Medicine, Shel with Tshawa-suum paste. The reduction in severity of langshu skin lesions following the treatments is similar to a finding in China, where herbal decoction and herbal ointment was found effective for chronic eczema [5]. A study among Langshu patients with purgation treatment in Tibet in 2017 showed that, the purgation helps in expelling the causes of langshu out of the body (ཚད་རྙིངས་དང་ཆུ་སེར་སོགས་ནད་རྒྱུའམ་སྙིགས་རོ་རྩ་ལྟོའི་གང་གི་བུ་གར་དྲངས་ཏེ་ཕྱིར་འབྱིན་པའམ་སྦྱོངས་བར་བྱེད་པ་ཡིན།) [10].
The ingredients of the Shel with Tshawa-suum paste, such as chetsha and durjed, contain anti-septic, anti-pyretic and anti-tumour properties [11]. The antiseptics are effective for the skin diseases such as atopic eczema [12]. One of the main ingredients in the Shel therapy is aru ra (Terminalia chebula), which contains antibacterial, antioxidant, antiviral and antifungal properties. Other ingredient such as emong (Clematis acutangular), somaraza (Abelmos moschatus), shrikhenda (Euphorbia royleana) and dongroe (realgar) contains the potency to cure imbalanced chuser (serum) and prevent unwanted serous fluid accumulation [13].
Location and severity index of skin lesion
Eczema is most commonly seen on the lower extremities, followed by the upper extremities and trunk [14]. In adults, lesions of eczema is common on the elbows, knee flexures, wrist, and ankles [15]. Similarly, Langshu is found more frequently on lower limbs and upper limbs, especially in young adults aged 18 – 39 years, who expose their limbs more than elderly people.
Most patients with Langshu are farmers, which could be due to their exposure to heat, cold, dust, and physical work. Sowa Rigpa text claims that thripa disorders are caused by physical work such as carrying loads and digging ground (མི་ཐེག་ཁུར་དང་ས་སྲན་བརྐོས་པ་དང་།།བང་དང་འགྲོ་ལས་དག་གིས་ཉེན་པ་དང་།།) [16].
A study on eczema in United Kingdom, with 25 children recruited to assess the association between trigger factors and disease flares in atopic eczema found that sweating, hot and damp weather were associated with disease flares in atopic dermatitis [17].
This study is the first of its kind in assessing the effectiveness of Shel with Tshawa-suum paste in the treatment of Langshu conducted in the Bhutanese Traditional Medicine system. Patients included in the study are normal day to day patients visiting the hospital and not from samples recruited through selection criteria. Therefore, the cases of Langshu diagnosed and treated by the Shel and Tshawa-suum reflect the real-life situation rather than experimented samples.
However, as the study coincided with the COVID-19 pandemic, there were travel restrictions that prevented a bigger sample size. Studies on skin diseases with larger sample size and longer period of time for follow-up and with controlled group is strongly recommended.
CONCLUSION
The administration of Shel (purgation) with Tshawa-suum (herbal medicine paste) resulted in the reduction of the size and severity of skin lesion in Langshu.
Declarations
Ethics approval and consent to participate
Ethics approval for this study was granted by Interim Institutional Review Board, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan, vide approval no. INTERIM IRB/PO20/022/454 dated 24th September 2020. Administrative clearance was obtained from the Medical Superintendent of NTMH. The permission to use EASI score tool was obtained from Wiley Global Permission. Informed consent was obtained from all the patients before the collection of data.
Consent for publication
Not applicable
Competing interests
None
Funding
There was no funding for this article.
Availability of data materials
All public sources of data have been cited in this article.
Author contributions
Conceptualization, data curation, formal analysis, methodology, resources,
writing – review and editing: SW, NL, TT, UW
Investigation, software, validation, visualization, writing – original draft: SW
Received: 28 February, 2024 Accepted: 09 April, 2024 Published online: 16 May, 2024
References
- Ministry of Health. Annual Health Bulletin 2020.Thimphu: Ministry of Health, Royal Government of Bhutan; 2021.
- Tsenam T. Gso rig rgyud bzhi’i’ grel chen drang srong zhal lung Vol. 3. 2000. pp. 140-143,108,43.
- བསམ་གཏན་. གསོ་རིག་སྙིང་བསྡུས་སྐྱ་རེངས་གསར་པ། དེབ་༢་པ་. ལྷ་ས་: བོད་ལྗོངས་མི་དམངས་དཔེ་སྐྲུན་ཁང་།; 2007.
- Tan HY, Zhang AL, Chen D, Xue CC, Lenon GB. Chinese herbal medicine for atopic dermatitis: A systematic review. J Am Acad Dermatol. 2013;69: 295–304. doi:10.1016/j.jaad.2013.01.019
- Prasad, Sai; Tomar, Rinku; Singh, Harbans; Sannd, Rajesh; Kumar S. Evidence based clinical practices in Vicharchika (Eczema) and Ayurvedic treatment modalities- Review. Int J Ayurvedic Med. 2019;11: 30–36.
- Tshenam T. Gso rig rgyud bzhi’i’ grel chen drang srong zhal lung Vol. 4. 2000.
- Tenzin KN. SI TU SMAN BSDUS E WAM. Two formularies of medical, magical and religious preparations. 1973.
- National Traditional Medicine Hospital. Standard Operating Procedue for shel therapy. 2019.
- Zhao CY, Tran AQT, Lazo-Dizon JP, Kim J, Daniel BS, Venugopal SS, et al. A pilot comparison study of four clinician-rated atopic dermatitis severity scales. Br J Dermatol. 2015;173: 488–97. doi:10.1111/bjd.13846
- མཚོ་སྔོན་སློབ་ཆེན་བོད་ལུགས་གསོ་རིག་སློབ་གླིང་གི་ཤེས་རམས་ཞིབ་འཇུག་སློབ་མའི་མཐར་ཕྱིན་དཔྱད་རྩོམ།. ལས་ལྔའི་ལོག་གནོན་རྩ་སྦྱོང་གིས་པགས་ནད་གླང་ཤུ་བཅོས་པའི་ནད་ཐོག་ཕན་སྐྱེད་ཞིབ་འཇུག. 2017; ༦༧-༡༠༣.
- Wangchuk P, Samten, Ugyen. High Altitude Medicinal Plants of Bhutan: An Illustrated Guide for Practical Use. Thimphu: Pharmaceutical and Research Unit; 2009.
- Lee M, Van Bever H. The role of antiseptic agents in atopic dermatitis. Asia Pac Allergy. 2014;4: 230–40. doi:10.5415/apallergy.2014.4.4.230
- སྨན་པ་ཚུལ་ཁྲིམས་སྐལ་བཟང་།. བོད་ཀྱི་གསོ་རིག་དང་ཨ་ཡུར་ཝེ་དྷ་ཀྲུང་དབྱིའི་སྨན་གཞུང་བཅས་ལས་བསྟན་པའི་སྐྱེ་དངོས་སྨན་རྫས་ཀྱི་དཔར་རིས་དང་ལག་ལེན་གཅེས་བཏུས།. Tshering P, Norbu T, Jamtsho, editors. རྒྱ་གར།: Materia Medica Department, Men-Tsee-Khang; 2008.
- Jiamton S, Tangjaturonrusamee C, Kulthanan K. Clinical features and aggravating factors in nummular eczema in Thais. Asian Pacific J allergy Immunol. 2013;31: 36–42.
- Weller R, Hunter J, Savin J, Dahl M. Clinical Dermatology. 4th ed. Blackwell Publishing; 2008.
- Y 19 Yonten Gonpo. The Root Tantra and The Expalanatory Tantra from the Secret Quintessential Instructions on the Eight Branches of the Ambrosi Essence Tantra. 2nd ed. Men-Tsee-Khang; 2011.
- Langan SM, Bourke JF, Silcocks P, Williams HC. An exploratory prospective observational study of environmental factors exacerbating atopic eczema in children. Br J Dermatol. 2006;154: 979–980. doi:10.1111/j.1365-2133.2006.07153.x
