Thinley Dorji1 ,
Jamyang Yeshi Dorji2
,
Jamyang Yeshi Dorji2 , Tempa Gyeltshen2
, Tempa Gyeltshen2 , Sangay Wangdi2
, Sangay Wangdi2 ,
Karma Tenzin3
,
Karma Tenzin3
1Department of Internal Medicine, Central Regional Referral Hospital, Gelephu, Bhutan
2Faculty of Traditional Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan
3Faculty of Postgraduate Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan
Corresponding author: Thinley Dorji, Department of Internal Medicine, Central Regional Referral Hospital, Gelephu, Bhutan.
Email: drthinleydorji@gmail.com
DOI: https://doi.org/10.47811/bsj.0012050814
Copyright © 2025 Bhutan Sorig Journal published by the Faculty of Traditional Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan.
This is an open access article under the CC BY-NC-ND license.
Health research is important for knowledge generation, evidence-based clinical practices, and data-driven policy decisions. Traditional Medicine (TM) is a form of knowledge accumulated over thousands of years and is based on textual descriptions, oral materials, and observations. Over the past decades, there has been growing interest in the field of research with the adoption of modern methods.
One of the first steps was implementing health research capacity-building activities across the TM sector [1]. Health research is taught to the students during their five-year undergraduate training and academic thesis is an integral component of postgraduate training. There have been ongoing continuing medical education activities on research methodology and statistics given to in-service health practitioners. Health research capacity-building activities conducted by the Ministry of Health or the Khesar Gyalpo University of Medical Sciences have involved members from the TM sector.
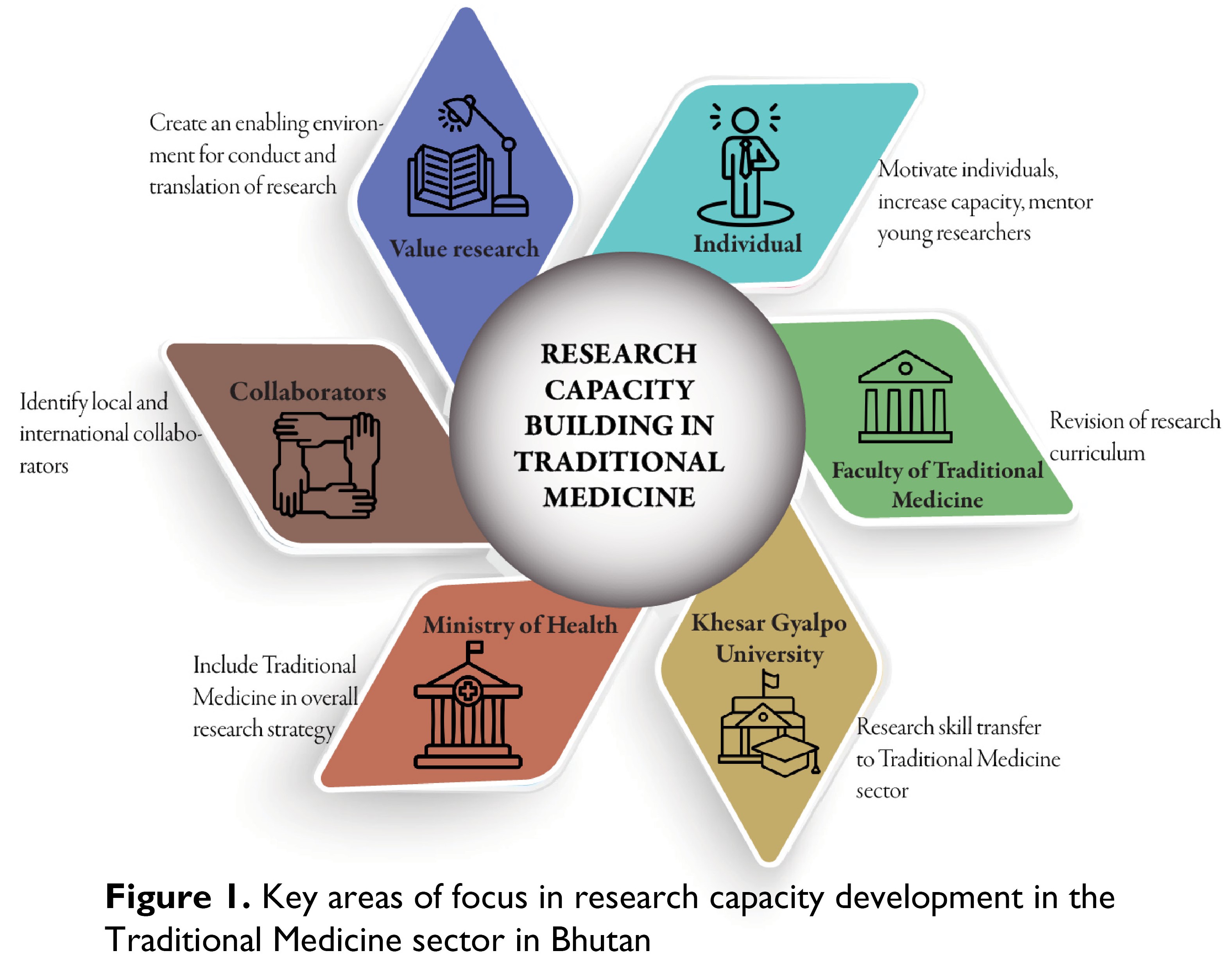
In Bhutan, the TM sector has major opportunities in health research including drug discovery, therapeutic efficacy of TM formularies and physical methods, and an opportunity for integration of TM in the overall care processes of patients. However, many challenges need to be addressed in improving the health research output in the field of TM in Bhutan (Figure 1). This article identifies the key players and their roles in the development and steering of TM research in the country.
The Faculty of Traditional Medicine has included health research methods in both undergraduate and postgraduate curriculum. However, there have been major challenges in its implementation due to the lack of an adequate number of faculty members to provide research training and supervision. For the postgraduate trainees, research training and evaluation are often coupled with the Faculty of Postgraduate Medicine. The curriculum for undergraduate training needs the adoption of practical health research and critical appraisal skills to enhance productivity in the field. Given the small pool of research teachers available at the Faculty, it is recommended to develop closer coordination with other faculties, in using resources for research training. Strong commitment and leadership in research capacity development are essential in building institutional capability.
Research teaching can become more effective if teaching faculty members are actively engaged in conducting research. Research publications have now been made an important criterion for academic promotions at the University. While there has been a gradual increase in the overall research output in TM, there are additional efforts required to generate research output across all fields of TM. One of the common reasons cited is a lack of research capacity despite having received research training workshops. This indicates the need for continued research mentorship required for the teaching faculty with strategic plans to graduate from the mentorship program through practical hand-holding experiences. The University should create avenues for customized research capacity building in the TM sector given its unique background and should actively encourage cross-faculty collaborations and sharing of expertise.
The field of Traditional Medicine or Sowa Rigpa goes beyond mere clinical practice and health services provided within the TM Units. It involves the provision of holistic care to the patients, including psychological and spiritual therapies. An important aspect is the involvement of TM practitioners in the identification of herbal or mineral components of medicinal/therapeutic formularies, involvement in the processes of production of medicines, and dispensation of these medicines/therapies. These components require collaboration and expertise involving biochemistry, phytochemistry, geochemistry, physiology, botany, and zoology. The impact of climate change on the availability of both high- and low-altitude medicinal plants requires major exploration with an overall aim of sustainability of plant material sources of medicines. Therapeutic testing and evaluation require clinicians, trialists, pharmacologists, and statisticians to conduct well-designed clinical trials and platform trials [2]. Comparative studies require close collaboration with allopathic practitioners to design studies that fill the evidence gap. An overall research institution may be established in the country with facilities for molecular testing, measurement of drugs or therapeutic targets, and testing in animal models.
As the scope of research expands in the TM sector, appropriate safeguards must be put in place for the protection of research subjects, including animal models, and the sharing of biomaterials across borders [3]. This requires strengthening the two ethics review boards, one at the Ministry of Health and the other at the Khesar Gyalpo University. As the country does not have a clinical trial registry, a policy document should be in place to mandate registration in any WHO-affiliated registry. One of the barriers faced in the field of research is the longer time required for obtaining these regulatory and ethics approvals. To create an enabling research ecosystem, all efforts must be made to improve the efficiency of these processes while maintaining the standards and requirements.
For research in TM to be driven by demand to answer clinically relevant and context-specific problems, there should be the adoption of evidence-based practices across all fields. Prioritization of research areas should involve service providers, policy-makers, patients, and independent thinkers. Although the principles of TM are driven by texts and oral transmissions, every clinical problem is a subject of research to find its relevant place in the overall patient care processes. For example, TM has been integrated as a part of palliative care medicine in Bhutan [4]. However, TM practitioners involved in the palliative care team should identify how best to utilize their position in the care team and generate evidence if this should be a global best practice.
This calls for the final question of why health research is needed. Apart from knowledge generation, knowledge should translate to better life, better patient outcomes, and better health system performance. Bhutan has a very unique health system that is fully funded by the government, and TM services are fully integrated with the health system. The study of health system function, health economics, and health policies related to TM in Bhutan is a unique area of research exploration. As much as the health system has strengthened TM, it is time for the TM sector to provide solutions for strengthening and sustaining the health system. Some areas of research, such as drug discovery and development of pharmaceutical herbal products have the potential not only for solving local problems but also filling in the critical knowledge gaps for the global population.
The TM sector is at a stage where it would benefit from collaborations in capacity building, institutionalization of research culture, and translation of research findings. Other Faculties within the University may provide exchange teaching and research skill transfer. Key areas of collaborative work require expertise that is available with international partners. In such areas, international well-wishers and collaborators are welcome for joint research projects and research capacity-building initiatives.
One of the key drivers of research capacity development is valuing research for excellence at individual, organizational, and institutional levels. The Sorig Conference is one platform where TM research is discussed and disseminated. The new evidence should be critically appraised and adopted in clinical and policy decision-making processes wherever possible.
In conclusion, the TM sector faces a unique set of challenges and opportunities in health research capacity development. We recommend the development and implementation of a strategic plan that is aimed at improving capacities at the level of students, individuals, institutions, and the TM system involving all relevant stakeholders and collaborating partners.
Declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
TD, JYD, TG, and KT are editors of this journal. All were blinded from the peer review process of this article.
Funding
There was no funding for this article.
Availability of data materials
All public sources of data have been cited in this article.
Author contributions
Conceptualization, investigation, resources, writing – original draft, writing – review and editing: TD, JYD, TG, SW, KT
Received: 30 September, 2024 Accepted: 16 October, 2024 Published online: 11 November, 2024
References
- Phuntsho S, Wangdi S. Research Seminars at the Faculty of Traditional Medicine, Khesar Gyalpo University, 2021-2023. Bhutan Sorig J. 2024;1: 53–55. doi:10.47811/bsj.0007050327
- Burki T. Platform trials: the future of medical research? Lancet Respir Med. 2023;11: 232–233. doi:10.1016/S2213-2600(23)00052-8
- Gurung MS, Dema T, Pelzom D, Tobgay T, Drukpa P. Research Ethics Board of Health: a seven year review of the only ethics review board in Bhutan. Bhutan Heal J. 2016;2: 18–22. doi:10.47811/bhj.18
- Laabar TD, Saunders C, Auret K, Johnson CE. doi:10.47811/bhj.18 Palliative care needs among patients with advanced illnesses in Bhutan. BMC Palliat Care. 2021;20: 8. doi:10.1186/s12904-020-00697-9
