Ugyen Chophel1 , Kuenga Sonam2
, Kuenga Sonam2 , Thinley Dorji3,4
, Thinley Dorji3,4 , Phuentsho5,
, Phuentsho5,
1Wangdue Hospital, Wangdue Phodrang, Bhutan
2Kidu Medical Service Centre, His Majesty’s Secretariat, Thimphu, Bhutan
3Department of Internal Medicine, Central Regional Referral Hospital, Gelephu, Bhutan
4Faculty of Postgraduate Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan
5National Biodiversity Centre, Ministry of Agriculture and Livestock, Serbithang, Thimphu, Bhutan.
Corresponding author: Ugyen Chophel, Wangdue Hospital, Wangdue Phodrang, Bhutan.
Email: Email: uchophel.96@gmail.com
DOI: https://doi.org/10.47811/bsj.0010050403
Copyright © 2025 Bhutan Sorig Journal published by the Faculty of Traditional Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan.
This is an open access article under the CC BY-NC-ND license.
ABSTRACT
Rhododendron toxicity can be life-threatening or fatal when manifested with cardiovascular and neurological adverse effects. A 56-year-old woman presented with dizziness, chest tightness, shortness of breath, and a tingling sensation in her face and limbs after ingestion of dried flowers of Rhododendron. On examination, she had sinus bradycardia and hypotension. She was admitted for monitoring and observation. She was managed with intravenous crystalloids, noradrenaline infusion, and atropine. Her vital parameters were normalised and was discharged after 24 hours. These symptoms were most likely due to grayanotoxin found in the Rhododendron species. This case highlights the need to raise awareness on the risks of plant poisoning due to rhododendrons and to seek timely medical care in case of symptoms. Clinicians are recommended to take context-specific history to identify potential aetiologies of poisoning.
Key words: Bradyarrhythmia; Grayanotoxin; Hypotension; Plant Poisoning; Rhododendron
INTRODUCTION
Poisoning is a process of detrimental effect that occurs following exposure to a foreign chemical substances or xenobiotics [1]. Poisoning is one of the common presentations to emergency departments of hospitals and requires early recognition and treatment to prevent mortality [2].
Poisoning is a significant global public health issue leading to considerable morbidity and mortality [2, 3]. The World Health Organization estimated that in 2019, there were 84,278 deaths worldwide Phuentsho5and a loss of five million disability-adjusted life-years due to unintentional poisonings [3]. In South Asia, the death rates from unintentional poisonings have seen a downward trend over the last three decades, declining from 986.2 per 100,000 in 1990 to 661.3 per 100,000 population in 2019 which was mainly due to improved access and availability of health care facilities [3]. The agents that are commonly reported in accidental poisoning are pesticides and drugs [1] and events of poisoning due to plants and plant products remain underreported. In Bhutan, there were 249 cases of poisonings reported with various agents in 2023 [4] and a few cases of aconite poisoning were admitted and managed at the National Referral Hospital [5]. However, there is a lack of a systematic reporting system for cases of poisoning and a lack of a technical centre to provide advice on the management of poisoning cases in the country.
Bhutan, often referred to as the land of medicinal herbs, has diverse plants being used as ingredients by local healers and Traditional Medicine practitioners [6]. Among the plants, most Rhododendron species that belong to the family Ericaceae are used in Traditional Chinese Medicine for the treatment of arthritis, acute or chronic bronchitis, asthma, pain, common cold, skin ailments, and gastrointestinal disorders [7, 8] and flowers of some Rhododendron species are traditionally used for nutritional purposes like making pickles, juice, jam, syrup, honey, squash, etc [8]. Bhutan is home to 46 out of more than 1000 Rhododendron species documented so far [12, 13]. It is available abundantly at altitudes between 2500 m to 4700 m above sea level [13]. Its flower blooms from April to July among different species across different altitudes when it is used for various purposes like medicine, altar offering and beautification. In Bhutan, a 3-day Rhododendron Festival is celebrated at Lampelri Recreational Park annually since 2013 to exhibit the flowers and shoots [14].
Rhododendron ingestion in large amounts is known to cause toxicity, owing to grayanotoxin. Intoxication in humans is reported following ingestion of rhododendron honey, dried rhododendron flower, and medicinal preparation in China, Nepal and the Black Sea region in Turkey [7-11]. Rhododendron toxicity can be fatal or life-threatening and manifests with various gastrointestinal, cardiac, and central nervous system symptoms. Here, we present a case of rhododendron toxicity in a middle-aged woman following ingestion of dried flowers to treat her indigestion.
CASE PRESENTATIONPatient Information
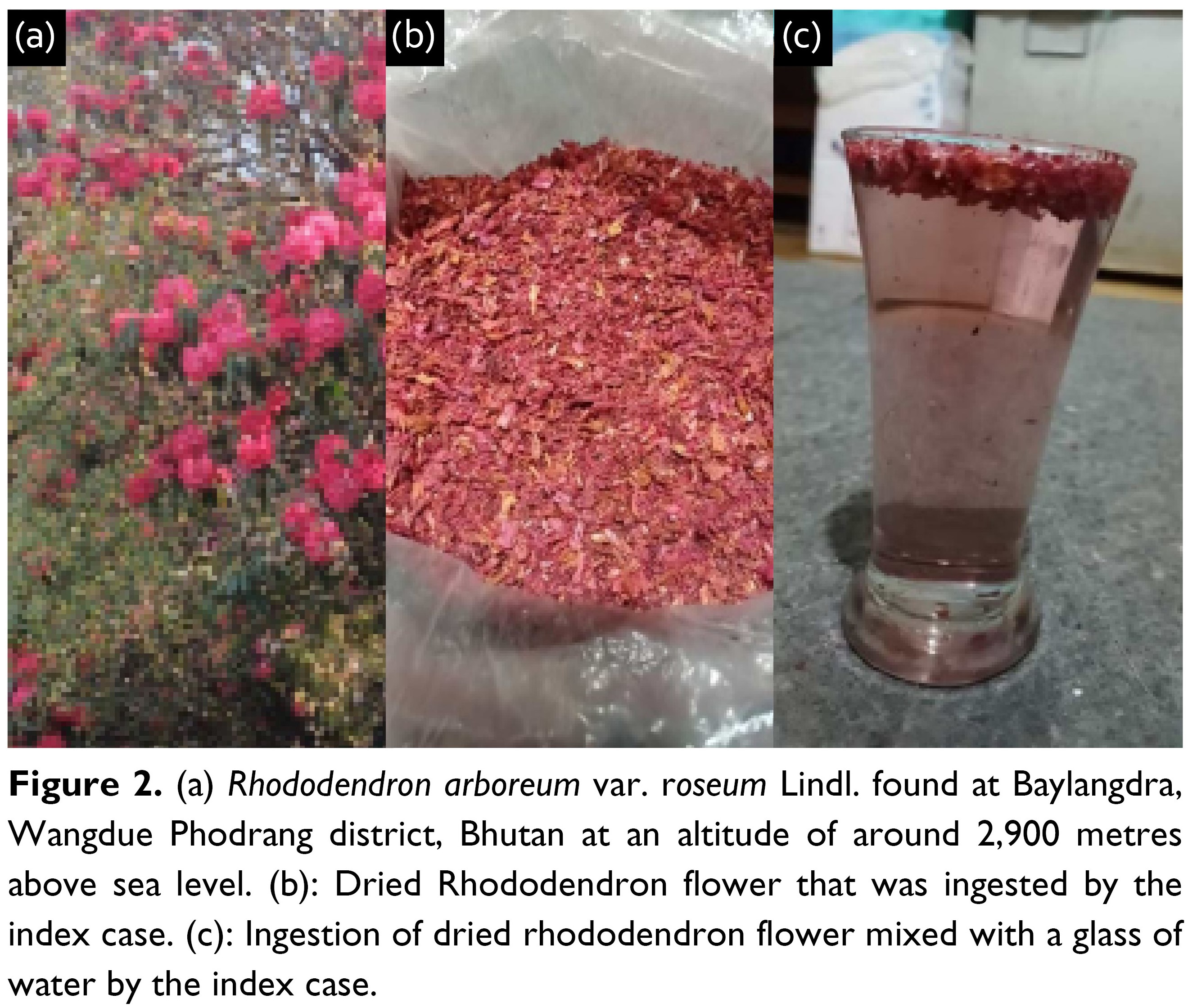
A 56-year-old female with no known comorbidities, who was residing at one of the temples in Baylangdra, Wangdue Phodrang was brought by ambulance to the emergency department of Wangdue Hospital with the complaint of persistent dizziness lasting 6 hours. She had an acute onset of dizziness following ingestion of a dried rhododendron flower of an amount of 50 – 100 g by mixing it with water and had three glasses of an amount of 600 mL. She had intentionally taken it to improve her indigestion issue after getting information from friends. She had other symptoms like nausea, anorexia, chest tightness, shortness of breath, and a tingling sensation in her limbs and face which all appeared 30 minutes after ingestion. She didn’t have vomiting, diarrhoea, seizure, and loss of consciousness. Because of persistent symptoms, she called Helpline 112, and she was picked up by an ambulance. At presentation, she had persistent dizziness, episodic chest tightness, and shortness of breath.
Clinical findings
On examination, the patient was conscious and well-oriented, Glasgow Coma Scale of 15. Her pulse rate was 50 beats per minute, regular; blood pressure was 90/44 mmHg, respiratory rate 18/minute, and SpO2 97% at room air. Clinical examination revealed no skin rash, tremor, or fasciculation. There was no murmur or gallop rhythm, the chest was clear with no added sounds, the abdomen was soft with no tenderness, and neurological examination showed no focal deficits.
Diagnostic assessment
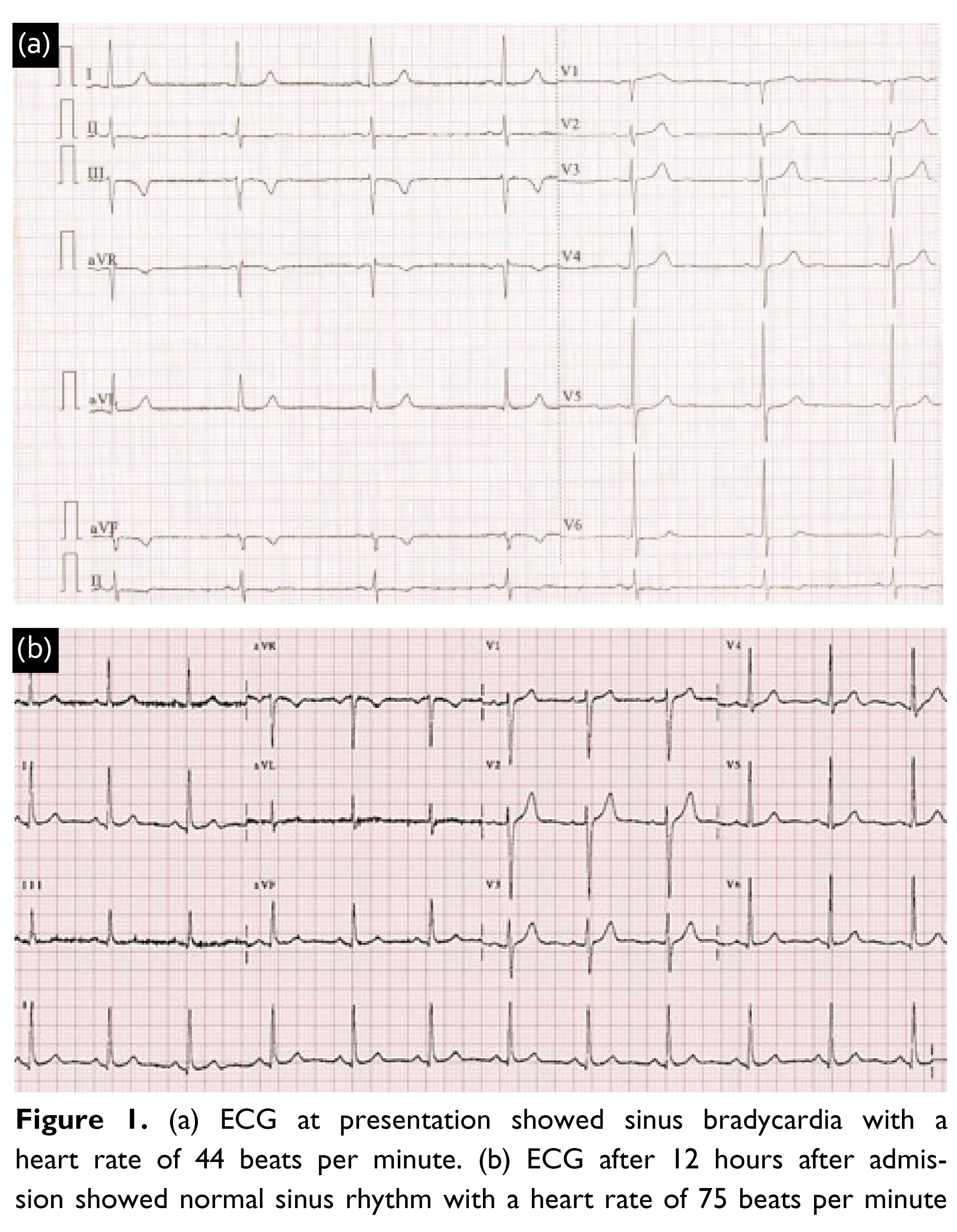
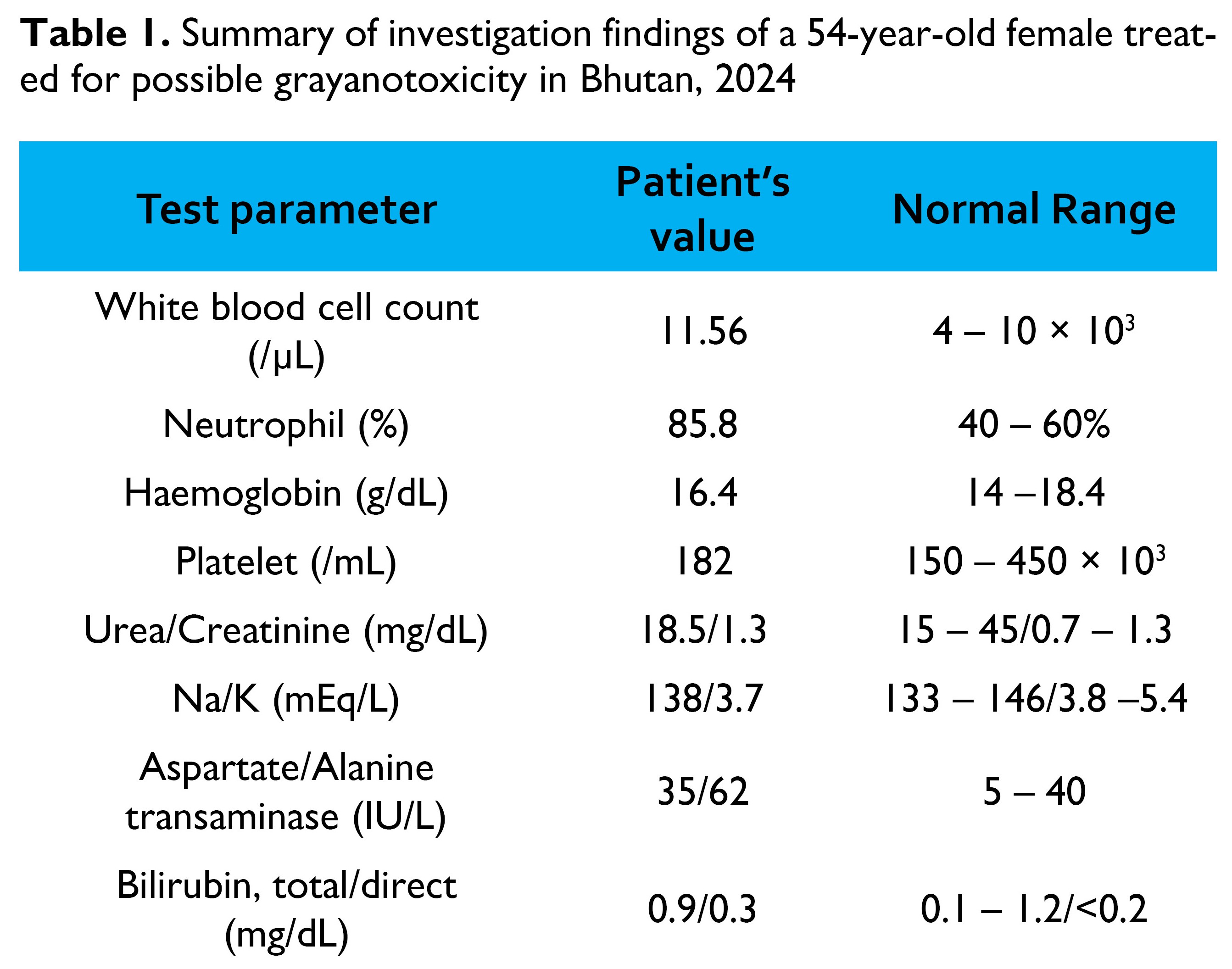
An electrocardiogram (ECG) showed sinus bradycardia with a heart rate of 44 beats per minute and T wave inversions in inferior leads with ST-segment changes (Figure 1a). Her initial complete blood counts, renal function, liver function, and electrolytes were unremarkable (Table 1). Her attendant displayed photographs depicting the dried rhododendron flower petals that were ingested, along with how it was consumed (Figure 2a). According to the clinical information, acute intoxication by rhododendrons was suspected. Using the Flora of Bhutan [12], the plant species was later identified as Rhododendron arboreum var. roseum Lindl. (Figure 2a) that is commonly called Eto meto in Dzongkha, Zhu dang metog in Tshangla, and Gurass or Gurans in Lhotshamkha.
As the patient was having symptomatic bradycardia, our differential diagnoses were myocardial infarction, dyselectrolytemia, accidental/unintentional ingestion of drugs like beta-blockers, calcium channel blockers, and aconite or rhododendron flower.
Intervention and outcome
Initially, hypotension was treated with the crystalloid bolus of 20 mL/kg (1500 mL) over 30 minutes. Her heart rate improved but due to persistent hypotension, she required noradrenaline infusion at 0.1 mcg/ kg/min. Her blood pressure was stabilized with vasopressor support but she had persistent bradycardia over 10 minutes in between and was treated with one dose of intravenous atropine (1 mg). Since then, her heart rate has remained above 60 beats per minute and her systolic blood pressure was above 90 mmHg. Following stabilization, she was transferred to the Medicine Ward for close monitoring and continued with intravenous crystalloids at 60 mL/hour. After 6 hours, vasopressor support and fluid were tapered off and she was observed for another 6 hours. She showed gradual improvement in her clinical condition with a heart rate of 75 beats per minute and blood pressure of 118/74 mmHg. An ECG done 12 hours after admission showed normal sinus rhythm with a heart rate of 75 beats per minute (Figure 1b). She was discharged in good health without any clinical symptoms after 24 hours of monitoring.
DISCUSSION
The genera Rhododendron, Agarista, Kalmia and Pieris which belong to the Ericaceae (heath) family contain grayanotoxins which are also known as andromedotoxin, acetylandromedol, or rhodotoxin. More than 20 isomers of grayanotoxin are isolated from rhododendrons [9]. Grayanotoxin 1 was identified from Rhododendron simsii in an infant presenting with toxicity in Hong Kong [11]. Grayanotoxin 1 and 2 have been found in the honey, leaves, and flowers of Rhododendron ponticum and Rhododendron flavum as reported in multiple case reports in the eastern Black Sea area [9, 10]. Grayanotoxin 1 is the principal toxic isomer that is responsible for the majority of the symptoms [9].The new shoots of Rhododendron arboreum are known to be poisonous to cattle [13]. Vegetative parts of Rhododendron thomsonii are also used as natural insecticides [14, 15]. The leaves and stamens of Rhododendron cinnabarinum are also poisonous to cattle.
The grayanotoxins bind to voltage-gated sodium channels preventing their inactivation. Excitable tissues like nerve and muscle cells, are thus maintained in a state of depolarization, and entry of calcium into the cells is facilitated resulting in negative chronotropic and ionotropic effects. The action is similar to aconitum alkaloid or aconite poisoning [9, 11]. It has adverse effects on cardiovascular symptoms like bradycardia, hypotension, and atrioventricular block. A case report about dried rhododendron flower ingestion by a man presenting as bradycardia and hypotension is reported in Nepal where it was managed conservatively with atropine and crystalloids[9]. Other symptoms of rhododendron poisoning include dizziness, chest tightness, shortness of breath, anorexia, nausea, vomiting, tingling sensation of face and limbs, muscular discomfort, blurred vision, convulsion, and loss of consciousness. A case report on poisoning from Rhododendron simsii in an infant in Hong Kong presented with a sudden onset of seizures, bradycardia, hypotension, and excessive salivation [11]. The occurrence of seizure is related to hypocalcemia resulting from its intracellular shift.
The mainstay treatment of this rhododendron toxicity is only supportive therapy including crystalloids and vasopressor infusion for hypotension and atropine sulphate for bradycardia. The prognosis is good and can recover within 24 hours [9, 11].
Key features of grayanotoxin toxicity include bradyarrhythmia, hypotension, and loss of consciousness in the background of consumption of rhododendron flower. However, not all rhododendron species are toxic; chemical analysis needs to be done for confirmation due to the risk of human poisoning. In this case, laboratory confirmation of serum levels of grayanotoxin could not be done due to a lack of appropriate facilities. As plant poisonings are a preventable cause of morbidity and mortality, it is important to create public awareness regarding the consumption of rhododendron products as home remedies.
Prevention of poisoning is one of the important indicators of the Sustainable Development Goals; a dedicated poison centre may be established to provide technical expertise for both clinical management and for creating public health awareness [2]. In addition, laboratories to identify and measure such poisons in vitro and in vivo may help in providing a wider understanding of the biochemical basis of such plant poisonings.
CONCLUSION
Poisoning with grayanotoxin in Rhododendron can be life-threatening, owing to its cardiovascular toxicity. This patient presented with symptomatic bradycardia and hypotension due to grayanotoxin after consumption of dried rhododendron flowers. While this patient had an uneventful recovery, it calls for the need to raise public awareness of rhododendron toxicity when consumed in excessive amounts.
Acknowledgement
We thank the patient and relatives for providing photos of the rhododendron tree and its flowers.
Declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Research Ethics Board for Health, Ministry of Health of Bhutan. Ref.No. /PO/RL/2024.2.NNW. Approval Date: 08-05-2024. Informed written consent was obtained from the patient.
Consent to participate
Informed written consent was obtained from the patient according to the consent process of the Research Ethics Review Board, Ministry of Health. No information related to patient identity or photos leading to the identification of the patient is presented.
Competing interests
TD is a member of the editorial board of this journal. TD was blinded and excluded from the peer review process of this article.
Funding
There was no funding for this article.
Availability of data materials
All public sources of data have been cited in this article.
Author contributions
Conceptualization, methodology, investigation, resources, writing – original draft: UC, KS, TD, P
Supervision, writing – review & editing: UC, TD
Received: 04 May, 2024 Accepted: 10 May, 2024 Published online: 16 May, 2024
References
- Sharma A, Patel S, Maiti A, Mishra A. An Epidemiological Study of Poisoning: A Follow-up Study from a Tertiary Care Hospital. J Prim Care Spec. 2024;5: 54–58. doi:10.4103/jopcs.jopcs_40_23
- World Health Organization. Guidelines for establishing a poison centre. Geneva: World Health Organization; 2020.
- Khan NU, Khan U, Khudadad U, Ali A, Raheem A, Waheed S, et al. Trends in mortality related to unintentional poisoning in the South Asian region from 1990 to 2019: Analysis of data from the Global Burden of Disease Study. BMJ Open. 2023;13. doi:10.1136/bmjopen-2022-062744
- Ministry of Health. Annual Health Bulletin 2023. Thimphu: Ministry of Health, Royal Government of Bhutan; 2024.
- Tshering U, Levine S, Watts M. Hypotension, bradycardia and reversible conduction defect induced by prescription of Bhutanese traditional medicines. Bhutan Heal J. 2018;4: 43–45. doi:10.47811/bhj.68
- Wangchuk P, Tobgay T. Contributions of medicinal plants to the Gross National Happiness and Biodiscovery in Bhutan. J Ethnobiol Ethnomed. 2015;11: 1–12. doi:10.1186/s13002-015-0035-1
- Popescu R, Kopp B. The genus Rhododendron: An ethnopharmacological and toxicological review. J Ethnopharmacol. 2013;147: 42–62. doi:10.1016/j.jep.2013.02.022
- Kumar V, Suri S, Prasad R, Gat Y, Sangma C, Jakhu H, et al. Bioactive compounds, health benefits and utilization of Rhododendron: A comprehensive review. Agric Food Secur. 2019;8. doi:10.1186/s40066-019- 0251-3
- Baral S, Baral BK, Sharma P, Shrestha SL. Dried rhododendron flower ingestion presenting with bradycardia and hypotension: a case report. J Med Case Rep. 2022;16. doi:10.1186/s13256-022-03413-8
- Jansen SA, Kleerekooper I, Hofman ZLM, Kappen IFPM, Stary-Weinzinger A, Van Der Heyden MAG. Grayanotoxin poisoning: “Mad honey disease” and beyond. Cardiovascular Toxicology. 2012. pp. 208–215. doi:10.1007/s12012-012-9162-2
- Poon W, Ho C, Yip K, Lai C, Cheung K, Sung R, et al. Grayanotoxin poisoning from Rhododendron simsii in an infant. Hong Kong Med J. 2008;14: 405–7.
- Grierson, A.J.C & Long D. Flora of Bhutan. Edinburgh: Royal Botanic Garden Edinburgh; 1991.
- Pradhan R. Wild Rhododendrons of Bhutan. 1999.
- Bhattacharyya D. Rhododendron Species and Their Uses with Special Reference to Himalayas-A Review. Biol Environ Sci. 2011;7: 161–167.
- Sikkim Bioinformatics Centre. Medicinal Plants. 2007.
